III. GENERAL PRINCIPLES OF ANESTHESIA
AIRWAY MANAGEMENT
Click the links below to access content on each subject area pertaining to Airway Management.
QUESTIONS
QUESTIONS
QUESTIONS
QUESTIONS
QUESTIONS
QUESTIONS

- The adult should be able to open his/her mouth so that there is at least three large fingerbreadths between upper and lower incisors.
- Mallampati 1: soft palate, fauces, uvula, anterior & posterior tonsillar pillars.
- Mallampati III: soft palate, base of uvula.
- The grade/assessment of only visualizing the epiglottis and not the glottic opening is a Cormack and Lehane III.
- The Interincisor gap is the assessment area is associated with the 3-3-2 airway rule.
- Temporomandibular joint mobility is best evaluated by having the patient open his/her mouth as wide as possible. Arthritis is the usual cause of temporomandibular joint immobility. Condylar head motion correlates with TMJ mobility.
- The adult should be able to open his/her mouth so that there is a 4 cm distance (three fingerbreadths) between upper and lower incisors. Atlantoaxial joint mobility is normally 35 degrees.
- The posterior cricoarytenoids are the laryngeal muscles responsible for opening the vocal cords.
- The lateral cricoarytenoids are the laryngeal muscles that adduct the vocal cords.
- The cricothyroid is an intrinsic muscle of the larynx is innervated by the external branch of the superior laryngeal nerve.
- The superior laryngeal artery supplies the supraglottic region of the airway.
- The primary function of the larynx is to protect the lungs from aspiration.
- The structure that divides the upper and lower airway is the cricoid cartilage.
- The internal branch of the superior laryngeal nerve provides sensory innervation above the vocal cords.
- The recurrent laryngeal nerve provides sensory innervation below the vocal cords.
- There are 9 cartilages in the larynx.
- There is 1 complete cartilaginous ring in the trachea.
- The left mainstem bronchus is 5 cm from the carina.
- Spinal nerves C3- C4- C5 supply the diagphragm.
- Independent risk factors for difficult mask ventilation show
- BONES (beard, obese, no teeth, elderly, snoring)
- Beard, BMI ≥ 26, edentulous, elderly, snoring
- Patients with Down’s syndrome may be difficult intubations d/t large tongue, short neck, small mouth, and subglottic stenosis; neck flexion during laryngoscopy and intubation may result in atlanto-occipital (cervical spine) dislocation because of congenitally weak ligaments; and irregular dentition.
- Rheumatoid arthritis patients have cervical spine involvement, TMJ synovitis, cricoarytenoid arthritis manifested by hoarseness, pericarditis, aortic regurgitation, pulmonary fibrosis, peripheral nerve compression, hepatitis, anemia, and drug-induced side-effects associated with aspirin and/or steroid therapy.
- Ankylosing spondylitis is a chronic inflammatory disorder that primarily affects the spine and sacroiliac joints and produces fusion of the spinal vertebrae and the costovertebral joints. Management of the upper airway is the priority because of the potential for obstruction. Cervical spine involvement may result in limitation of movement.
- Cervical spinal cord injury should be assumed to be present in any patient who has sustained trauma to the head or face, in any unconscious trauma patient, and in any patient who complains of pain before or after careful palpation of the cervical spine.
- Treacher Collins is a condition that can result in upper airway obstruction due to the underdevelopment of the tongue, maxilla, and/or mandible.
- Optimal intubation requires aligning the oral, laryngeal, and pharyngeal axes for proper sniffing position.
- Direct visualization of the laryngeal inlet with the endotracheal tube positively identified in it is the most reliable method of verification. ETCO2 with capnograph/mass spectrometer also provides reliable evidence of tracheal rather than esophageal intubation.
- A miller blade provides a direct view of the vocal cords by lifting the epiglottis.
- An indication for awake intubation is a known history of difficult intubation. Also, morbid obesity creates several factors that make intubation difficult (short, muscular neck; inability to visualize uvula). Contraindications to fiberoptic bronchoscopy: hypoxia; thick airway secretions; airway bleeding; local anesthetic allergy; and unable to cooperate.
- A patient who is ready for extubation should have a spontaneous breathing rate less than 30 per minute. Also, the pH should be within the normal range (7.35- 7.45), PaCO2 35- 45, and zero PEEP.
- The trigeminal nerve block is utilized to prevent nasal pain associated with awake intubation.
- To block the posterior 1/3 of the tongue, the glossopharyngeal nerve is anesthetized.
- A transtracheal block is performed after the needle is placed and air is aspirated.
- Correct application of cricoid pressure is the application of 4 kg of force.
- With the difficult airway, preoxygenation (actually denitrogenation) is an essential component to delay arterial desaturation during subsequent apnea. It increases the oxygen content and eliminates much of the nitrogen (79% of room air) from the functional residual capacity (FRC). Without preoxygenation (denitrogenation), the oxygen reserve in the FRC will last approximately 2.5 minutes in a can’t ventilate/can’t intubate situation. With good preoxygenation, the FRC has enough oxygen to last almost 12 minutes. Adequate preoxygenation should include having the patient breathe at normal tidal volumes for 3 to 5 minutes with a fresh gas flow of no less than 5 L and a tight mask fit. The respiratory bag should move with each inspiration/expiration, and there should be a good end-tidal CO2 waveform. This is easily accomplished by applying the face mask as soon as the patient arrives in the operating room before the application of other monitors. If time is limited, “fast-track” preoxygenation, in which the patient takes four vital capacity breaths in 30 seconds, can be used before induction of anesthesia. This does not completely denitrogenate the blood but is useful in the emergent situation. REWORD
- Full spontaneous recovery of train-of-four (4/4) can still mean 70% of receptors are blocked.
- LMAs should be avoided in parturients (lower esophageal sphincter tone relaxation), full stomachs (obvious risk to aspiration), and patients who cannot effectively communicate or follow instructions.
- The largest ETT size that an LMA Fastrach will allow is 8.5 mm in diameter.
- A safety feature of an endotracheal tube that allows for air to enter the trachea if the distal tip is occluded is called the Murphy’s eye.
- Pressure applied to the cricoid cartilage is known as Sellick’s maneuver.
- The purpose of the two vertical bars on an LMA Fastrach are to prevent obstruction of the ETT by the epiglottis.
- Both lean and obese people share the rate of preoxygenation.
- Head tilt and jaw thrust maneuver with positive airway pressure using 100% oxygen are maneuvers used to help break a laryngospasm.
- During an event where the glottis is occluded, such as laryngospasm or airway obstruction, a patient’s breath creates a more negative intrathoracic pressure. This pressure creates a shift in fluid from the blood to lungs, resulting in coarse breath sounds. NPPE is treated with increased FiO2/CPAP/PEEP.
- Risk factors include obesity (metabolic disorder and increased external abdominal pressure), diabetes (delayed gastric emptying), and GERD (decreased lower esophageal sphincter tone). Cricoid pressure is contraindicated with known cervical spinal injury.
- Succinylcholine is often utilized in rapid-sequence inductions due to its quick onset. However, it is also a known trigger of malignant hyperthermia. In this situation, rocuronium can provide onset of paralysis comparable to succinylcholine and it not a known trigger.
- Ludwig angina is an oropharyngeal example of airway obstruction.
- If the patient has received radiation treatment to the tumor, the obstructing mass may be stiff and friable, and furthermore, temporomandibular joint mobility may be compromised. In this case, a tracheostomy is preferable as attempts at intubation risk serious hemorrhage and edema which may lead to complete obstruction of the airway.
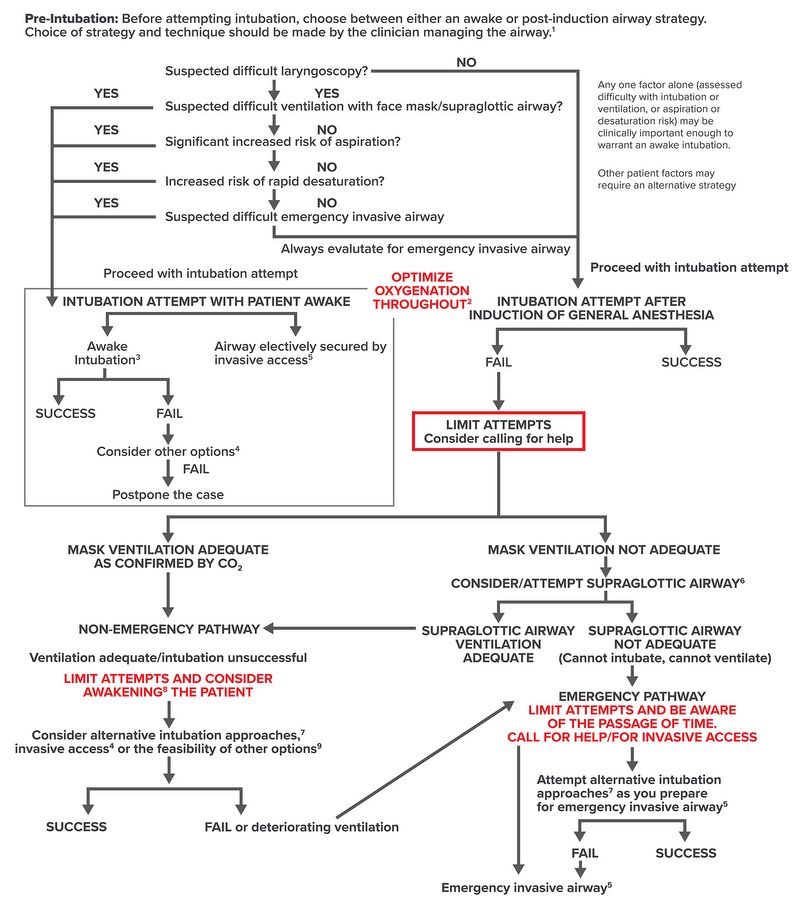
- Failed intubation
→ Mask ventilate (Adequate) → Non-emergency pathway
→ Mask ventilate (Inadequate) → Supraglottic airway
→ Supraglottic airway (Inadequate)
CANNOT INTUBATE/ CANNOT VENTILATE
Invasive access should be attempted
- After a failed intubation, the provider should first try to optimize oxygenation and mask ventilate. If mask ventilation is adequate, then a non-emergency pathway can be attempted. If unable to ventilate, the provider should attempt a supraglottic airway.
- When failed intubation and inadequate mask ventilation occurs, a supraglottic airway (e.g. LMA) should be attempted. If the LMA is inadequate, this is a CANNOT INTUBATE/CANNOT VENTILATE situation and invasive access should be attempted/considered.